Public discourse has recently surrounded protocols for breast screening in Canada and how the country approaches women’s breast health. This discussion was prompted by the release of the draft recommendations on screening for breast cancer by the Canadian Task Force on Preventive Health Care (CTFPHC) on May 30th.
The CAR guidelines are clear – breast cancer screening should start at 40. The draft recommendations put forth by the CTFPHC are a guide for women who are at average risk of breast cancer and are considering going through screening, typically those aged 40-75; they don’t apply to patients with a history of breast cancer, increased breast density, or those who show symptoms that are suggestive of breast cancer.
The CTFPHC outlines that breast cancer screening should be a personal choice for patients and they should be comprehensively informed of the benefits and harms of the screening process. The patient should be able to make an informed decision that aligns with their personal values. According to the Task Force, if the patient chooses to go forward with screening, they should be offered a mammogram every two to three years.
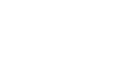
Upon release of the draft recommendations, the CAR responded with a statement that highlights several key points from the CAR’s own breast screening guidelines.
“The CAR has developed guidelines that recommend screening from age 40 using evidence-based data,” said CAR President Dr. Ania Kielar. “Currently, there is a severe shortage of human health resources, specifically technologists, including in mammography. We need to work together with Health Canada, other levels of government, and radiologists to continue to increase equitable access to breast imaging for women, particularly those at higher risk for cancer.”
Health Canada has since called a meeting of medical experts to gain insight and feedback, attended by Dr. Kielar and breast health expert Dr. Rachel Fleming. “Health Minister Mark Holland was keen to hear more from experts in breast imaging to further his understanding of the limitations of the Task Force recommendations and was very open to feedback,” said Dr. Kielar. “Dr. Fleming succinctly explained the CAR's position about the need to increase access to imaging for women, including those 40-50 years old, and the urgency to increase person-power in the form of technologists and health human resources.”
Dr. Fleming is a member of the CAR’s Breast Imaging and Intervention Working Group. She believes it is productive to have discussions whenever new guidelines come out, as it allows stakeholders to critique the authors and test the veracity of the recommendations. “Everyone involved in the recommendations or subsequent discussions wants to make sure women get appropriate care. That’s the place we are all starting from.”
She says that recommendations should ultimately help referring physicians know what to do in a way that is easily accessible and not overwhelming. She noted that the messaging of these recommendations could be clearer, saying it could be easy to glean that the Task Force doesn’t want to screen patients at all, which is an incorrect interpretation.
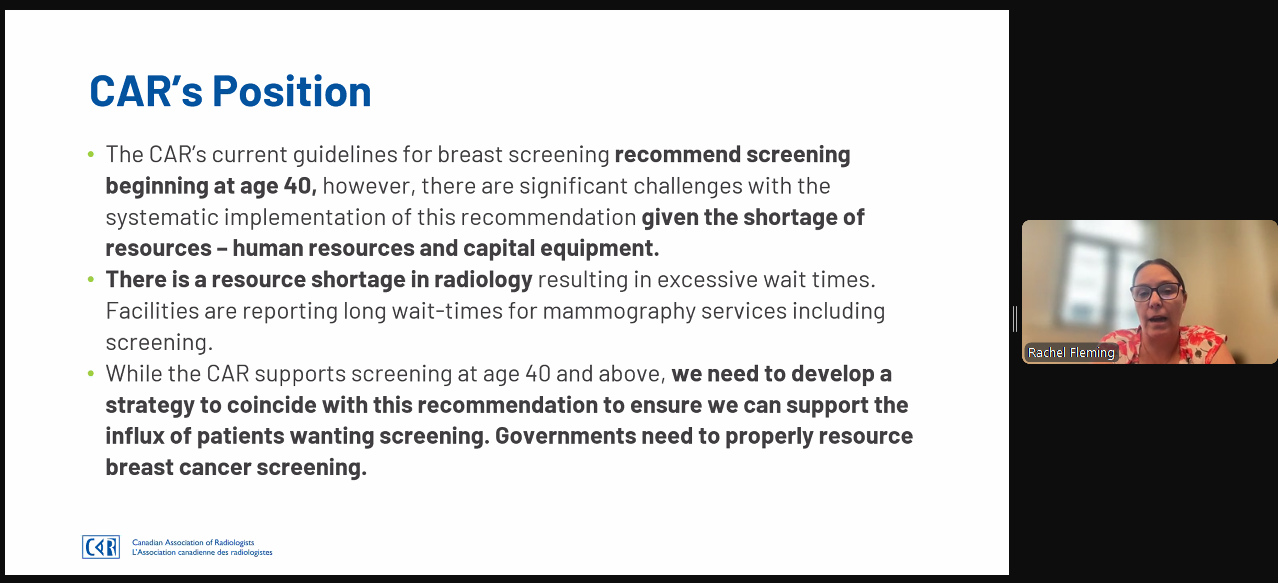
On Thursday, June 27, the CAR partnered with the Canadian Cancer Society (CCS) to present a joint webinar covering the main tenets of the recommendations and an overview of the Task Force. The CAR is recognized as the national voice of radiologists, and it is important for the organization to take a leadership role in conveying the meaning and purpose of the recommendations, says Dr. Fleming.
“The vast majority of breast reporting is done by general radiologists. It is critical to make sure they are aware of the status of the recommendations and are kept up to date as they are communicating with referring physicians. Everything needs to be done with the aim of finding the appropriate test for the appropriate patient.”
The public is encouraged to share their feedback with the CTFPHC on their draft recommendations until July 11.