Financing models for healthcare are evolving, with greater emphasis now being placed on value. How does radiology fit into this equation and how can we be certain that its value is maximized? Representatives from the CAR contributed to a multi-society[1] expert statement published in the CARJ and other journals in December 2020 that outlines the value contributed to healthcare by radiology, and explains how value may be measured, recognized, and augmented. Here we summarize the key points and offer a Canadian perspective on that international publication, Radiology in the Era of Value-Based Healthcare: A Multi-Society Expert Statement From the ACR, CAR, ESR, IS3R, RANZCR, and RSNA.
Key Points
- Value-based healthcare (VBH) is a framework for improving individual patient health outcomes per unit of expenditure.
- Radiology is a key component of healthcare and has a significant impact on patient outcomes; it must be considered a vital element of VBH.
- By embracing VBH principles, radiology can contribute to moving to a value-driven system, where all investigations or interventions contribute positively to patient outcomes.
VBH is about demonstrating improved patient outcomes while considering all of the inputs involved. Just like “beauty is in the eye of the beholder,” the definition of value varies depending on your perspective and assigned measures. Patients, providers, and administrators each have a unique perception of value and will place variable weight on the factors that feed into value, namely quality, service, and cost.
“In the future, healthcare institutions will likely be encouraged to implement and demonstrate the use of VBH principles and optimal resource utilization to ensure continued funding. It is incumbent that radiologists have a better understanding of the theories and assumptions underlying VBH,” said Dr. Richard Walker, CAR’s Lead Representative on the Conference Board of Canada’s Centre for Value-Based Healthcare Canada.
In his seminal 2010 NEJM paper outlining the VBH model, economist Michael Porter writes, “Value should always be defined around the customer, and in a well-functioning healthcare system, the creation of value for patients should determine the rewards for all other actors in the system.”
The CAR recognizes the integral role of radiology in modern medicine, and the centrality of medical imaging to diagnosing and treating disease across the continuum of care and all patient demographics. Unfortunately, Porter’s framing of VBH does not account for the value of radiology, despite the long-term and system-wide cost savings and benefits to patient outcomes associated with short-term spending on radiology.
Radiology – a source of value creation
It is crucial that we ensure radiology is appreciated not as a potential driver of healthcare cost, but as a source of value creation. The authors of the statement suggest this can be done by quantifying radiology’s impact on patient outcomes and on measurements used historically by policymakers and other third-party payers, such as Quality Adjusted Life Years (QALYs) and Incremental Cost Effectiveness Ratio (ICERs).
Pathways exist for radiologists to demonstrate meaningful contributions to patient health outcomes, or to have their funding/reimbursement influenced by value-based activities, such as shifting emphasis to readability of reports, following up on incidental findings, and engaging on quality metrics.
Value metrics
- Precise, reproducible, and measurable imaging-specific and clinically relevant metrics linked to agreed and important health outcomes.
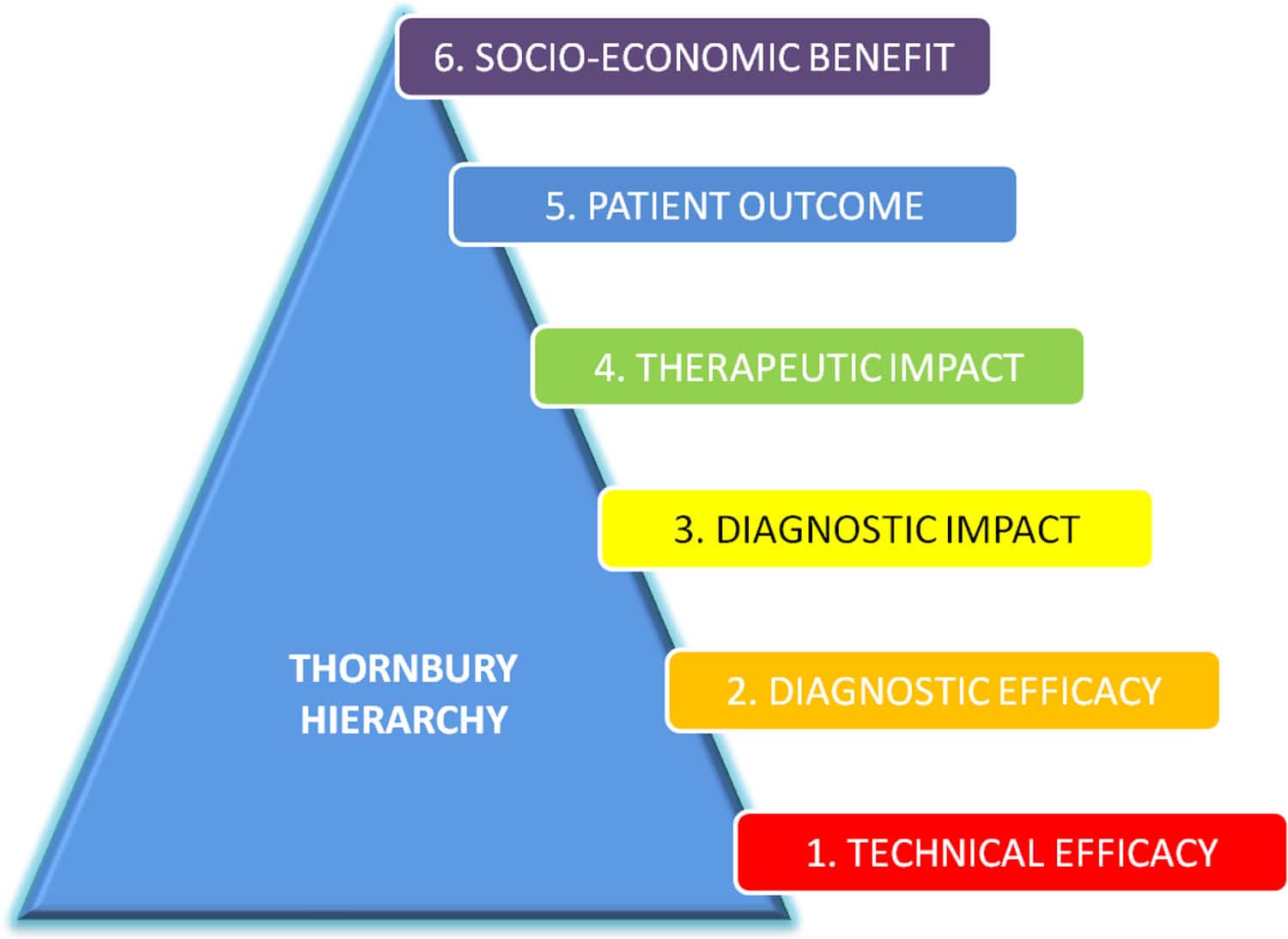
- Higher level outcomes including socio-economic benefit (see figure). For example, while a diagnostic test such as breast MRI, performed using the same equipment, scanning parameters, and interpreter, may have equivalent diagnostic performance in two different patient groups, its efficacy will likely be greater in women with specific characteristics (e.g. BRCA1 mutation carriage).
- Process metrics to measure aspects of value delivery including timeliness of information delivery, application of appropriate levels of specialization to interpretation, and tailoring of information delivery to the needs of different types of intermediate customers (e.g. emergency care, primary care, non-urgent specialty care).
- Traditional radiology research metrics like diagnostic and technical accuracy may be sufficient to demonstrate a value contribution for tests and procedures with smaller, well-defined target populations and/or clear impacts on patient outcomes (levels 1 and 2 of the Thornbury Hierarchy), but we also need to address the higher levels of the scale (levels 3-6) by developing robust, reproducible, and clinically relevant outcome metrics to objectify and quantify the value contributed by radiology at the societal level.
Referral Guidelines – a CAR led initiative
The CAR is currently undertaking a national project on referral guidelines that will help demonstrate the value of radiology for the healthcare system in a holistic, concrete, and measurable way. With support from the Canadian Medical Association (CMA), the CAR will develop referral guidelines for medical imaging to support referring physicians in selecting the best imaging tests for their patients. We will make these evidence-based, peer-reviewed guidelines freely available and will promote their use by developing clinical decision support (CDS) systems.
Value-Based Healthcare Canada
Another mechanism by which the CAR is helping to demonstrate the value of radiology at the national level is by engaging with the Conference Board of Canada’s Centre for Value-Based Healthcare Canada. Dr. Richard Walker (University of Calgary) represents the CAR on the Centre’s membership. The Centre was established to formalize an infrastructure that will serve to advance the implementation of VBH approaches in Canada. Building on the Value of Radiology, Part II report by the Conference Board of Canada, we will continue to position the economic benefits of investing in medical imaging equipment, infrastructure, technology, and health human resources, in a clear and balanced way.
Please contact the CAR if you are interested in getting involved.
[1] Drs. Emil Lee, Josephine Pressacco, and Richard Walker are the authors associated with the CAR. Two of the paper’s authors, Drs. Adrian Brady and James Brink, discuss the paper in an RSNA podcast from March 2021.